Clinical Pharmacology of Intravitreal Aflibercept
The clinical efficacy of intravitreal anti-VEGF drugs has been widely demonstrated in several angiogenesis-driven eye diseases including diabetic retinopathy, diabetic macular edema, and the neovascular form of age-related macular degeneration. Pegaptanib, ranibizumab, and aflibercept have been approved for use in the eye, whereas bevacizumab is widely used by ophthalmologists to treat patients “off-label”.
However, these drugs are active in the nanomolar to picomolar range; Despite the small doses used for eye diseases and the intravitreal route of administration may limit systemic side effects, these drugs can penetrate utilizing the blood circulation and alter systemic VEGF with unknown clinical consequences, particularly in vulnerable groups of patients.
Clinical pharmacokinetics of ocular anti-VEGF agents should therefore be taken into account when choosing the right drug for the individual patient.
The gaps in current understanding that leave open important questions are as follows: (i) uncertainty about which drug should be given first, (ii) how long these drugs can be used safely, and (iii) the choice of the best pharmacological strategy after first-line treatment failure.
Diabetic Retinopathy
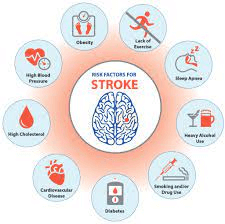
Diabetic retinopathy (DR) is a leading cause of blindness worldwide. Its severity ranges from nonproliferative DR (NPDR) to proliferative DR (PDR), The microvascular ischemia associated with DR leads to vision loss, primarily through pathologic neovascularization of the retina and/or anterior segment and diabetic macular edema (DME). Increasing NPDR severity is associated with an increased risk of progression to PDR and vision loss.
Research report on the use of Aflibercept for severe NPDR
Research has evaluated vascular endothelial growth factor blockade therapy with intravitreal aflibercept injections in eyes with severe NPDR without diabetic macular edema (DME) and ave seen that a proactive treatment of nonproliferative diabetic retinopathy (NPDR) with intravitreal aflibercept reduces the risk of progression to vision-threatening complications.
Generally, Intravitreal injections of a vascular endothelial growth factor (VEGF) inhibitor reduced disease severity and imaginative and prescient-threatening issues in sufferers with severe nonproliferative diabetic retinopathy (NPDR),
Retina upon treatment with use of aflibercept
Intravitreal alibercept is used in the retina.
It was recorded that after 1 year of medication with aflibercept (Eylea) in an eye with severe NPDR, approximately eighty% of patients who obtained a greater intensive dosing regimen noticed a two-step or enhanced improvement within the Diabetic Retinopathy Severity Scale (DRSS)
Once PDR has developed, retinal damage from fibrosis and contraction may additionally now not be reversible, even with intervention, and can be associated with permanent vision loss,
“Subsequent remedy with [panretinal photocoagulation] ends up invisible field loss because the procedure is inherently destructive. Hence, prevention of progression to PDR and DME becomes a clinical issue of concern.
FDA approved Intravitreal Aflibercept (Eylea) in 2019 as indicated to treat all tiers of diabetic retinopathy and diabetic macular edema. The VEGF inhibitor, which works utilizing blocking off the boom of new blood vessels and lowering vascular permeability, also holds signs for neovascular age-related macular degeneration and macular edema following retinal vein occlusion.
Dose and Dosage
For diabetic retinopathy, the suggested dose is 2 mg (0.05 mL) of intravitreal injection every four weeks for the first 5 injections followed via 2 mg via intravitreal injection as soon as every 8 weeks.
Despite the fact no new safeguard indicators emerged, essentially the most general ocular antagonistic pursuits — taking place in 7.5% of eyes in any trial arm — covered conjunctival hemorrhage, DME, vitreous floaters, and eye ache. There have been no cases of endophthalmitis.
As a result, however, 1 year of aflibercept therapy greatly diminished the occurrence of PDR and CI-DME.
Hence the management of severe non-proliferative diabetic retinopathy with intravitreal aflibercept injection improved the severity of retinopathy and reduced the risk of progression to Centre-involved diabetic macular edema (CI-DME) and vision-threatening complications.
Nonproliferative DR could serve as a potential window of opportunity to slow disease progression, thereby preventing the development of potentially irreversible damage that may lead to vision loss and have a meaningful impact on quality of life.
Treatment at a fixed interval may be an optimal strategy compared with reactive PRN dosing. Fixed intravitreal aflibercept injection dosing in a patient population who adhered to the treatment regimen was demonstrated to be safe and effective in preventing vision-threatening complications and Centre-involved diabetic macular edema (CI-DME) in eyes with severe NPDR; Neverthelessemploying, The drug is better used for a longer-term follow-up of this approach may be insightful.
Read more on: