Why Eye Evaluation?
The primary care physician frequently encounters patients with ocular symptoms and signs that may signal serious underlying systemic disorders. In such cases, the Ocular manifestation of systemic disease as obtained from an ocular examination may aid in the diagnosis and management of the underlying systemic disease. Alternatively, patients known to have systemic diseases may develop ocular problems that require the attention of an eye care profession. For these reasons, the primary care physician should be familiar with the common ocular complications of frequently encountered systemic diseases as there often ocular manifestation of systemic diseases. And as well encourage for regular routine eye evaluation and check.
To provide a framework for approaching ocular manifestations of systemic disease, there is need for ocular evaluation or eye evaluation.
This program is organized according to these list of systemic diseases with ocular manifestation:
- Congenital,
- Traumatic,
- vascular,
- neoplastic,
- autoimmune,
- idiopathic,
- infectious,
- metabolic/endocrine, and
- drugs/toxins.
To avoid overlooking pathology of the eye in systemic diseases, it is important that the primary care physician or Optometrist considers performing an eye examination for each patient. The complete eye evaluation should include:
1. Visual acuity
2. External examination (lids and orbit)
3. Pupils (including assessment for relative afferent pupillary defect)
4. Motility examination
5. Examination of anterior segment (conjunctiva, sclera, cornea, anterior chamber, and lens)
6. Dilated ophthalmoscopy
7. Visual fields Patients with visual symptoms need an ophthalmologic referral because ocular findings such as anterior chamber inflammation, corneal dendrites, or retinal pathology can be easily missed.
In addition, there should be due considerations of eye diseases and treatment options to save sight.
OCULAR MANIFESTATION OF CONGENITAL DISORDERS
Ocular manifestation is a feature of numerous congenital syndromes, including Down syndrome, Marfan syndrome, myotonic dystrophy, tuberous sclerosis, metabolic disorders involving lysosomal storage and carbohydrate metabolism, and neurofibromatosis. An ocular examination may provide key findings in an effort to establish a definitive diagnosis with key monitoring of ophthalmic manifestation in systemic diseases.
Examples of Congenital disorders with ocular manisfestations
Neurofibromatosis
Classical neurofibromatosis (NF1) is among the most common inherited disorders in humans, with an estimated incidence of 3 in 10,000.
The disease is characterized by
• 6 or more hyperpigmented skin macules (café-au-lait spots; see the slide, left)
• 2 or more cutaneous neurofibromata or 1 plexiform neurofibroma
• Melanocytic hamartomata of the iris (Lisch nodules; see the slide, right)
• Multiple “freckles” in the intertriginous areas
• Distinctive osseous lesions (eg, sphenoid dysplasia, pseudoarthrosis or thinning of the long bone cortex)
• Glioma of the anterior visual pathway
• Patient history of a first-degree relative with NF1 Ophthalmic manifestations of classical neurofibromatosis may commonly involve the eyelid, iris, orbit, and optic nerve.
The iris Lisch nodules may be one of the key signs in screening individuals. Ninety-five percent of individuals with NF1 will have Lisch nodules by the time they are 6 years old.
OCULAR MANIFESTATION OF TRAUMATIC DISORDERS
Shaken Baby Syndrome and the eyes
The shaken baby syndrome is increasingly evident in our society. Injuries in a child with a history that is not appropriate for the injury sustained should raise a suspicion of child abuse. Ocular manifestation of this syndrome can be detected with a dilated fundus examination may reveal form of preretinal, intraretinal (including white centered hemorrhages), or vitreous hemorrhages. Photographic documentation of retinal findings should be obtained immediately, as these findings may be fleeting.
OCULAR MANIFESTATIONS OF VASCULAR DISEASES
Systemic Hypertension
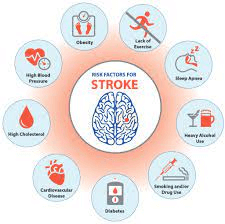
Systemic diseases such as hypertension is a cardio vascular disease that affect the retinal, choroidal, and optic nerve circulations. A variety of retinal vascular changes can be seen in this systemic disease; these depend in part on the severity and duration of the hypertension. Ocular manifestation of systemic diseases such as hypertension include retinal changes in form of flame-shaped hemorrhages in the superficial layers of the retina and cotton-wool patches caused by occlusion of the precapillary arterioles with ischemic infarction of the inner retina. Long-standing hypertension can produce arteriolar sclerotic vascular changes, such as copper or silver wiring of the arterioles, as shown by the two arrows on the right, or arteriorvenous nicking. Another ocular manifestation sign of chronic hypertension in the fundus of a hypertensive patient is lipid exudates resulting from abnormal vascular permeability, as shown by the arrow at left. More ominous in this photograph is swelling of the optic disc as its most common ocular manifestation, seen here by the blurring of the temporal disc margins. This is the hallmark of malignant hypertension, which carries a poor prognosis for the patient’s health if left untreated. BP must be emergently controlled to decrease the risk of developing heart and renal failure and hypertensive encephalopathy as well as stroke and permanent vision loss.
Embolic Disease
Emboli to the ophthalmic circulation can lodge in the ophthalmic artery or the central retinal artery, producing severe loss of vision that can be transient or permanent (left). In the elderly, the most common source of emboli is fibrin and cholesterol from ulcerated plaques in the wall of the carotid artery. The so-called Hollenhorst plaque is a refractile cholesterol embolus that lodges at an arterial bifurcation, as shown in the right-hand slide.
Emboli of cardiac origin may come from calcified heart valves in patients with a history of rheumatic fever, from an atrial myxoma, or from fibrin-platelet emboli in patients with mitral valve prolapse, as seen here in this left eye with superotemporal branch retinal artery occlusion. This is cholesterol based systemic disease with ocular manifestation.
Cholesterol emboli eye presents with sudden, persistent visual loss may be due to occlusion of the central retinal artery, and emergency ophthalmologic evaluation is indicated. Ophthalmoscopic examination will reveal narrowed retinal arterioles and a pale retina. Edema with loss of retinal transparency in all areas except the fovea gives rise to the appearance known as the “cherry-red spot” (left). All these ocular manifestation can be prevented if detected early. Compare that appearance with a normal fundus (right). Emergency treatment is directed to decreasing intraocular pressure and to vasodilation in an attempt to allow the obstructing embolus to pass into less critical, smaller-caliber vessels.
Other sources of emboli include talc in intravenous drug abusers, as seen here in the macula, and fat in patients with long bone fractures. Talc emboli do not typically cause occlusion or ischemia although rarely they may be associated with retinal neovascularization.
Central Retinal Vein Occlusion
Another cause of painless vision loss is a central retinal vein occlusion (CRVO). This vision loss may be mild to profound and is often due to macular edema. The onset of a CRVO is usually rapid. Ophthalmic examination will reveal retinal hemorrhages and cotton-wool spots. The findings of severe vision loss or an afferent pupillary defect indicate a greater risk for the ischemic type of CRVO, which carries a poor prognosis and is more highly associated with rubeotic glaucoma. Fifty percent of patients who have a CRVO have open-angle glaucoma and/or systemic hypertension. A systemic workup in patients with a CRVO should include measurement of blood pressure and exclusion of other vasculopathic risk factors. Blood workup to rule out coagulopathies (including Factor V deficiency), hyperlipidemia, collagen vascular diseases, and paraneoplastic syndromes may be considered.
Migraine: Ocular Migraine
Migraine is a transient vasospastic phenomenon affecting the cerebral and/or ocular circulations. Paroxysmal neurologic or visual symptoms include scintillations, amaurosis fugax, transient cortical blindness, and transient homonymous hemifield loss, which consists of nasal field loss in one eye and temporal field loss in the other. Migraine symptoms, which are presumably due to focal cortical or ocular ischemia, may last from 15 to 45 minutes.
In classic ocular migraines, these visual symptoms are followed by an intense, throbbing headache. Common migraine is a periodic headache of varying intensity without a preceding aura. Complicated migraine occurs when frequent severe migraine headache results in a persistent visual or other neurologic deficit. However, the visual phenomena may occur without headaches, which is called ocular or acephalgic migraine or migraine equivalent. A treatable vascular disease such as vasculitis or arteriovenous malformation needs to be considered in the differential diagnosis of acephalgic migraine.
The Migraine treatment depends on the frequency of the episodes and can be directed to preventing attacks rather than aborting them. Episodes that occur less frequently than once a month may not require treatment. Fortunately, the paroxysmal ocular phenomena rarely lead to permanent visual deficits, but patients with visual loss during attacks should probably have an ophthalmologic evaluation. Discontinuation of oral contraceptives should be considered, as they may trigger vascular occlusive disease in migraine patients.
OCULAR MANIFESTATION BLOOD DYSCRASIAS
A blood dyscrasia is any abnormal or pathologic condition of the blood. Ocular manifestation of blood dyscrasias include hyperviscosity syndromes, thrombocytopenia, and all forms of anemia, including sickle cell anemia.
Hyperviscosity Syndromes
Patients with such as polycythemia, multiple myeloma, dysproteinemia, and leukemia may present with visual complaints. These include amaurosis fugax and permanent visual loss.
Initial fundus changes are retinal vein dilation, retinal hemorrhages, and varying amounts of disc edema (as seen in this fundus).
Leukemia
Patients with leukemia may present with a hemorrhagic type of retinopathy, as seen here. Note both the retinal and the preretinal hemorrhages (see arrows). The hemorrhages are presumably due to thrombocytopenia of leukemia. White centered hemorrhages may indicate metastatic leukemic infiltration of the retina.
Direct leukemic infiltration of the optic nerve
Direct leukemic infiltration of the optic nerve can cause pronounced optic nerve swelling and vascular congestion with edema and hemorrhages of the surrounding retina, as seen here. This can rapidly lead to blindness if not treated promptly with radiation. Periodic dilated funduscopic examination is recommended for asymptomatic patients with hyperviscosity syndromes, and referral to an ophthalmologist is indicated if any ocular symptoms or signs develop.
Sickle Cell Anemia : How does sickle cell disease affcets the eyes
Sickle cell retinopathy occurs most frequently in the HbSC form of the disease but may also be seen in the HbSS form and in sickle thalassemia. Sickle cell retinopathy is not seen in patients with sickle cell trait only.
Sickling can produce retinal arterial occlusions, especially in the retinal periphery, as shown by the arrows in the slide (left). The retinal ischemia can lead to peripheral (“sea fan”) neovascularization (as seen in this slide, right), vitreous hemorrhage, and tractional retinal detachment. Panretinal laser photocoagulation may be necessary to expedite regression of the neovascular process. General anesthesia can produce sickling and thereby increase the risk of arterial occlusive disease. Sickle cell eyes treatment should begin with ophthalmologic evaluation because patients may be asymptomatic, even in advanced stages of the retinopathy, due to the peripheral location of the retinal changes, which can only be visualized via indirect ophthalmoscopy through a dilated pupil.
NEOPLASTIC EYE DISEASE: WHAT IS NEOPLASM IN THE EYE
The most common ocular tumors or type of intraocular malignancy in adults is metastatic carcinoma, arising from primaries in the breast or lung in women and in the lung in men. Patients are often asymptomatic but may present with decreased or distorted vision.
An easily detected iris mass is visible in this patient with metastatic lung carcinoma. An irregularly shaped pupil, iritis, or blood in the anterior chamber may signal a metastatic nodule, as seen here.
Choroidal metastases from breast cancer
Because of its rich vascular supply, the choroid is the most common site for ocular metastasis. Choroidal metastases may be solitary or multiple and may affect one or both eyes. Typically they appear as creamy-white lesions, as seen in this patient with metastatic breast cancer. Associated leopard spotting may also be detected. Choroidal metastases are often subtle and difficult to detect with direct ophthalmoscopy and may require referral to an ophthalmologist if suspected or if visual loss or visual distortion develops. Treatment options include local radiation and chemotherapy.
Because ocular metastases may represent the smallest clinically detectable lesions of disseminated carcinoma, an ophthalmologist monitoring these lesions at regular intervals may help to assess the efficacy of systemic treatment. However, prognosis for survival after detection of an intraocular metastasis is generally poor, with a mean length of survival of 6 to 9 months. Retinoblastoma is one of the most metastatic tumors of the retina.
AUTOIMMUNE DISORDERS THAT AFFECT THE EYES
Certain autoimmune disorders, such as connective tissue diseases, thyroid eye disease, and myasthenia gravis, can initially present with ocular manifestations only. Thus, it is extremely important for the primary care specialist to screen for those disorders in patients with the most common ocular symptom (dry eyes) so that these patients can receive the appropriate treatment as early as possible in the course of these diseases.
Ocular manifestation of Connective Tissue Disorders (Collagen Vascular Diseases)
Connective tissue disorders have various ocular manifestations, the most common being tear deficiency leading to dry eyes, or keratoconjunctivitis sicca. The symptoms of dry eyes include burning, a foreign-body or gritty sensation, and photophobia.
Sjögren’s syndrome, the complex of dry eyes and dry mouth, may occur in isolation or in association with a connective tissue disorder. Specific antibodies such as anti-SS-A (or antiRo) may be associated with Sjögren’s syndrome.
Artificial tears are the primary treatment for mild to moderate keratoconjunctivitis sicca. Generally, to be efficacious, they must be used several times a day on a regular basis. Numerous commercial preparations are available, and the patient’s preference is sometimes the best criterion for selecting a given agent. Patients with severe dry eyes or with sensitivity to preservatives should be steered to one of the preservative-free lanolin-free formulations. Nighttime administration of lubricating ointment may also be helpful. Occlusion of the lacrimal drainage puncta can aid retention of tears. Environmental modifications include humidifiers, goggles, and side shields on glasses. Recent advances demonstrate the efficacy of anti-inflammatory agents, administered in topical form.
Severe tear deficiency may be unresponsive to routine use of artificial tears and can result in corneal epithelial breakdown, ulceration, and even perforation, as seen here. Consultation by an ophthalmologist is indicated for patients with tear deficiency states who have persistent pain or visual loss.
Ankylosing Spondylitis: Does it cause uveitis?
Up to 25% of patients with ankylosing spondylitis have one or more attacks of iritis, a form of intraocular inflammation, which may precede the clinical arthritis. Patients typically present with ocular symptoms such as; photophobia, redness, and decreased vision. Patients with symptoms or signs suggestive of iritis (shown here) should be referred for evaluation by an ophthalmologist.
Iritis usually responds to treatment with topical corticosteroids and dilating agents. However, topical corticosteroids should be prescribed only with the advice of an ophthalmologist, because long-term corticosteroid therapy can lead to glaucoma, cataract formation, or exacerbation of ocular infections, and, in some connective tissue disorders, to ocular perforation.
Most common ocular manifestation in patients with Rheumatoid Arthritis
The ocular manifestation of rheumatoid arthritis are most often seen in patients with more active and severe forms of the disease and in those with extra-articular complications. Aside from dry eyes, other common ocular manifestations are inflammation of the episclera and sclera, peripheral corneal ulcers, and uveitis.
Episcleritis is inflammation of the superficial tissue overlying the sclera. Typically patients complain of mild to moderate pain and tenderness, and there is localized or diffuse redness of the eye.
Scleritis (inflammation of the sclera) may sometimes appear clinically similar to episcleritis. However, severe, deep pain is a distinguishing feature of scleritis.
Scleritis may be characterized by active inflammation with redness, as seen on the left, and severe pain. It can progress to necrosis, as seen on the right, and subsequent perforation of the sclera (necrotizing scleritis).
Scleromalacia perforans consists of scleral melting in a white, quiet eye. This condition also can lead to ocular perforation.
Peripheral corneal ulceration is another manifestation of rheumatoid arthritis that may result in ocular perforation. Patients with rheumatoid arthritis who develop peripheral corneal ulceration or scleritis have an associated risk for developing potentially lethal systemic vasculitis. Primary care physicians should monitor patients with active rheumatoid arthritis for symptoms and signs of episcleritis, scleritis, and corneal ulcers; patients who develop these ocular conditions should be referred to an ophthalmologist for treatment.
Juvenile Rheumatoid Arthritis
Ocular involvement in juvenile rheumatoid arthritis typically occurs in patients with a mild form of the disease, the so-called pauci-articular form, and in patients who are rheumatoid-factor negative and ANA positive. Ocular complications may occasionally be the presenting feature of this disease and do not correlate with the severity or course of the systemic signs. The characteristic triad of late ocular complications in juvenile rheumatoid arthritis consists of iritis, cataract, and, as seen here, band keratopathy, which consists of whitish deposits of calcium in the cornea. Band keratopathy is a late sequela of many forms of chronic intraocular inflammation. Iritis or iridocyclitis can occur in up to 15% of patients with JRA and causes few symptoms or signs. The iritis is usually chronic, causing secondary cataract formation and glaucoma. All patients with JRA should be screened and followed by an ophthalmologist.
Systemic Lupus Erythematosus
Patients with systemic lupus erythematosus (SLE) can have many of the same ocular manifestations associated with rheumatoid arthritis, such as dry eyes, scleritis, and peripheral corneal ulceration. The most common severe manifestations of SLE, however, involve the vasculature of the retina and optic nerve.
A variety of retinal complications can occur in SLE, including retinal vasculitis with cotton wool spots, as seen here, and hypertensive retinopathy secondary to renal involvement. Lupus anticoagulant or phospholipid antibody syndrome is a variant characterized by a higher incidence of thrombotic episodes, which may cause vascular occlusions and may require anticoagulant therapy.
Lupus vasculitis can also involve the optic nerve, resulting in ischemic optic neuropathy. Note the pale, swollen nerve in this young woman, who presented with visual loss due to ischemic optic neuropathy as the initial manifestation of SLE. Ophthalmologic evaluation is indicated for patients who have central nervous system involvement or visual symptoms. Detection of retinal vasculitis can also assist, in certain instances, in establishing the diagnosis of SLE.
Polyarteritis or Periarteritis Nodosa
This condition is a widespread inflammatory disease affecting small and medium-size blood vessels, most commonly in middle-aged men. In addition to dry eyes, the ocular manifestations are peripheral corneal ulceration, scleritis, associated hypertensive retinopathy, and primary retinal vasculitis similar to that seen in patients with SLE. Other connective tissue diseases associated with ocular inflammation are Reiter’s syndrome, Wegener’s granulomatosis, and Behcet’s disease. Wegener’s can be associated with anterior or posterior scleritis and/or retinal vasculitis including retinal vascular obstruction. The classic triad of Behcets includes hypopyon uveitis, arthritis and oral ulcers. Fulminant occlusive retinal vasculitis with progressive retinal necrosis may warrant aggressive immunosuppressant therapy.
Sarcoidosis
Sarcoidosis, a multisystem disorder of unknown etiology, is characterized in part by granulomatous inflammation of many organs. This disease more commonly affects the African-American and Hispanic populations. Ocular involvement occurs in about 25% of patients presenting with other features of sarcoidosis.
The most common ocular presentation is granulomatous uveitis, characterized in part by large clumps of cellular deposits on the endothelial layer of the cornea, which are called keratic precipitates (left).
Choroiditis and retinal vasculitis, usually segmental, may occur in a small percentage of patients. The typically gray, perivenous infiltrates are characteristically called “candlewax drippings” (right). Optic disc involvement is rare but may occur in patients with central nervous system involvement. Edema or granuloma of the optic nerve may be present.
Many of these changes are difficult to detect with direct ophthalmoscopy, and dilated ophthalmologic evaluation is indicated for all patients who have sarcoidosis with suspected ocular involvement. Treatment of the ocular problems is similar to treatment of the systemic disease and often includes the use of topical, injectable, or systemic corticosteroids.
Giant Cell (Temporal) Arteritis
Giant cell, or temporal, arteritis is a systemic vasculitis that usually affects people over age 60. Although almost any artery can be involved, this disease has a predilection for large and medium sized vessels, particularly the superficial temporal, ophthalmic, and proximal portion of the vertebral arteries. The symptoms include headache, scalp tenderness, jaw pain and difficulty in chewing (claudication), the polymyalgia rheumatica complex (myalgia, weight loss, anorexia, and fever of unknown origin), and acute visual loss. Palpation of the temporal artery may reveal tenderness, a lack of pulsations, and enlargement or nodular thickening of the vessel.
Ischemic optic neuropathy, or infarction of the optic nerve head, is the most common presentation of giant cell arteritis; it is associated with severe unilateral loss of vision, a relative afferent pupillary defect or Marcus Gunn pupil, and, as shown here, a pale, swollen optic nerve head.
Cranial motor nerve palsy is the initial ophthalmic presentation of giant cell arteritis in about 10% of patients; it is due to nerve ischemia resulting from occlusion of the vascular supply to the nerve. Most commonly, the third cranial nerve is affected, producing ptosis and outward deviation of the eye on the involved side (as seen here), with sparing of the pupil. In the elderly, a cranial nerve palsy should raise suspicion of giant cell arteritis, especially if accompanied by headache or pain.
If giant cell arteritis is suspected, a STAT erythrocyte sedimentation rate and c-reactive protein must be obtained, followed by a temporal artery biopsy. A low or normal sedimentation rate does not exclude this diagnosis, especially if the patient is taking nonsteroidal anti-inflammatory agents for other reasons. (Up to 20% may have a normal sedimentation rate.) Fluorescein angiography is a photographic test that can reveal characteristic deficits in the choroidal circulation of the eye. Histopathologic examination of the temporal artery typically reveals a patchy, granulomatous inflammatory reaction that involves the media and the adventitia of the artery.
A potentially blinding disease, giant cell arteritis usually affects the second eye in a matter of hours or days if untreated. Therefore, this condition is considered an emergency, and treatment must be initiated empirically without waiting for the laboratory results. Therapy consists of high daily doses of systemic corticosteroids, which are gradually tapered according to serial sedimentation rates and the patient’s symptoms, both of which are monitored closely. Recent studies suggest that there is a more rapid response if patients are begun on intravenous corticosteroids for 24 to 48 hours before switching to oral corticosteroids. Corticosteroids should be started before the biopsy, as biopsy results will not be affected for a number of days. Patients suspected of having giant cell arteritis are best managed jointly by the primary care physician, rheumatologist, and ophthalmologist.
Thyroid Disorders
Ocular abnormalities are common in patients who suffer from thyroid dysfunction. Thyroid ophthalmopathy is not always correlated with serum thyroid hormone levels and may occur even in patients who are euthyroid. It is important to remember that the eye disease may continue to progress after thyroid function tests have returned to normal. All of the ocular manifestations should be closely followed in conjunction with an ophthalmologist.
Thyroid eye disease can vary in its severity and presentation. It can involve the eyelids, orbit, extraocular muscles, cornea, conjunctiva, and optic nerve. Ocular involvement can be unilateral or bilateral.
Lid retraction causes the patient to have a widened palpebral fissure, as seen on the left. Sometimes the sclera is exposed above or below the corneoscleral limbus; this is termed scleral show. The patient on the right exhibits soft tissue involvement, with eyelid fullness and injection of the conjunctiva.
Thyroid ophthalmopathy can cause proptosis, or exophthalmos (left). The extraocular muscles can become enlarged secondary to lymphocytic infiltration. This can lead to diplopia from restriction of eye movements. The muscle most commonly affected is the inferior rectus muscle, which causes restriction on attempted up gaze (shown at right, in patient’s left eye).
In severe cases, vision loss can occur. Proptosis and lid retraction can lead to corneal damage, as seen on the left. Sight loss can also occur due to optic nerve compression. The optic disc may appear swollen, as in the clinical photograph on the right, or may be atrophic. In early stages of optic nerve compression, the optic nerve can appear normal.
In severe cases, vision loss can occur. Proptosis and lid retraction can lead to corneal damage, as seen on the left. Sight loss can also occur due to optic nerve compression. The optic disc may appear swollen, as in the clinical photograph on the right, or may be atrophic. In early stages of optic nerve compression, the optic nerve can appear normal.
Computed tomography of the orbit may demonstrate proptosis, as seen in the left scan, and extraocular muscle swelling or enlargement, as seen in both scans.
Thyroid ophthalmopathy typically occurs in two phases that should be jointly managed by the primary care physician and the ophthalmologist. The first phase is characterized by acute congestive changes and lasts an average of 2 years. Treatment in this phase is directed toward preserving sight and providing symptomatic relief. Medical treatment for corneal problems includes the use of tear substitutes in the form of drops or ointments. For the extraocular muscle or optic nerve involvement during the acute congestive phase, intermittent high doses of corticosteroids may be employed. If this therapy fails, orbital irradiation or surgical decompression may be required to save deteriorating vision.
The second phase is marked by cicatricial changes in the eyelids, extraocular muscles, or orbit. Treatment may consist of surgically correcting the ocular muscle deviation, the functional abnormalities, or the cosmetic deformities.
Myasthenia Gravis
Myasthenia gravis is a myopathy that may occur at any age. It is an autoimmune disease affecting the acetylcholine receptors, causing a conduction defect at the neuromuscular junction. About 75% of patients present with ocular manifestations, including bilateral ptosis (as seen in this patient), limited eye movements, and/or diplopia. Among these patients, approximately 20% will have only ocular manifestations. Any patients with ptosis and diplopia of unclear etiology, especially if variable and worsening with fatigue, should be presumed to have myasthenia gravis. Referral to a neurologist may be necessary because of systemic involvement, including apnea and choking due to involvement of respiratory and pharyngeal muscles.
IDIOPATHIC DISORDERS
Intracranial Hypertension
The most common ocular manifestation of intracranial hypertension is optic disc swelling, which in this condition is referred to as papilledema. The visual symptoms of papilledema are often mild or absent; the most common are transient visual obscurations, which can range from mild blurring to complete visual loss, usually lasting only a few seconds. Ophthalmoscopy typically reveals marked disc swelling and vascular engorgement, as seen here.
Common causes of intracranial hypertension include brain tumor, meningitis, venous sinus thrombosis, hydrocephalus and the entity pseudotumor cerebri, or idiopathic intracranial hypertension. Pseudotumor cerebri may be associated with vitamin A or vitamin D intoxication, tetracycline therapy, and steroid withdrawal. Pseudotumor cerebri has a propensity to occur in young, obese women, and in most cases a precipitating factor is not found. Disc edema can also be caused by conditions that are not associated with increased intracranial hypertension, such as sarcoidosis, syphilis, tumor, and pseudo-disc edema from causes such as optic nerve head drusen (shown).
Multiple Sclerosis
Within 5 years of an episode of optic neuritis, more than 40% of women aged 20 to 40 will manifest signs and symptoms of multiple sclerosis. Optic neuritis presents as an acute, painful vision loss in one or both eyes occurring over a few days to two weeks. It may be the initial manifestation of multiple sclerosis. After one episode, 70% of eyes with optic neuritis recover spontaneously within 3 to 6 months. The Optic Neuritis Treatment Trial demonstrated that patients treated with intravenous methylprednisolone, 250 mg every 6 hours for 3 days, followed by 1 day of oral prednisone, had a more rapid visual recovery than a placebo-treated control group. By 1-year follow-up, however, there was no statistically significant difference between the treated group and the control group. In addition to intravenous methylprednisolone, another medication that has been shown to be of benefit is interferon beta-1a. A multicenter trial of interferon beta-1a (Avonex) showed a reduction of recurrent MS attacks, slowing of cognitive deterioration, and lessening of disease activity, as measured by gadolinium-enhanced MRI.
INFECTIOUS DISORDERS
Acquired Immunodeficiency Syndrome (AIDS)
Dry eyes are very common in patients with AIDS, but they are a nonspecific finding. The three most common classic lesions are retinal cotton-wool spots, cytomegalovirus (CMV) retinitis, and Kaposi’s sarcoma of the eyelid or conjunctiva.
Cotton-wool patches, which are due to obstruction of the precapillary arterioles with infarction of the superficial retina, are the most common ocular finding in patients with HIV infection. Associated intraretinal hemorrhages may also be present and these findings are collectively referred to as HIV noninfectious retinopathy.
Patients with AIDS can develop infectious retinitis secondary to a variety of opportunistic organisms. Ocular manifestation of systemic diseases in HIV/AIDS patients, often come in form cytomegalovirus (CMV) retinitis, as seen in this patient, which is characterized by discrete, fluffy, white retinal necrotic patches with hemorrhages. Because cytomegalovirus retinitis can begin in the retinal periphery, patients with AIDS should be referred for ophthalmologic evaluation evaluation especially if symptomatic or with reduced T-cell counts.
CMV retinitis therapy has evolved significantly. The incidence of CMV retinitis has decreased tremendously with the advent of HAART (Highly Active Anti-Retroviral Therapy). If CMV retinitis is detected in a patient who is not on HAART, the patient must be immune reconstituted with anti-retroviral medications. Induction IV ganciclovir or foscarnet is also necessary, and intravitreal injections of ganciclovir may be considered. As cytomegalovirus infection is usually a systemic infection, intravenous therapy is usually the treatment of choice. The primary care physician and the ophthalmologist must work closely together to monitor efficacy of therapy and side effects of the treatment. As CD4 counts increase and viral load decreases to an acceptable level, IV and intravitreal ganciclovir administration may be withheld as long as the CD4 counts remain above 100. If patients develop CMV retinitis on HAART or have no response to IV therapy, then ganciclovir implants and intravitreal injections are necessary.
In patients with AIDS, opportunistic infections such as CMV retinitis occur predominantly when CD4 counts fall below 50 cells/ml. However, other retinal infections such as syphilis, toxoplasmosis, herpes simplex virus, or varicella-related retinitis (acute retinal necrosis syndrome) may occur in immunocompromised or immunocompetent eyes.
OCULAR MANIFESTATION OF METABOLIC/ENDOCRINE DISORDERS
Diabetes
Diabetes commonly produces significant ocular complications that may lead to blindness as an Ocular manifestation of systemic disease , if not recognized and treated. Diabetic retinopathy is now the leading cause of new blindness in adults aged 20–74 in the United States. Because of its ophthalmologic significance, diabetic retinopathy is covered in detail in Diabetes and Eye Disease, a separate educational program in this series, and is not discussed further here.
DRUGS/TOXINS
Ocular manifestation of systemic diseases could sometimes be as a result of the medications these patients take to treat the disease conditiion. Significant ocular side effects including vision loss can be caused by systemic medications, for example, toxic retinopathy can be caused by thioridazine, chloroquine, hydroxychloroquine, and tamoxifen, and toxic optic neuropathy can be caused by ethambutol, isoniazid, and fluoroquinolones.