Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19
The conditions of coronavirus infections have greatly affected all parts of the body which includes the eyes. Ocular signs and symptoms of presentation have been investigated to understand the mode of transmission of the virus across all eye tissues. The condition of Covid19 effect on the eyes spans across the uveitic, retinovascular and neuro-ophthalmic diseases. This makes a case for interprofessional team management of the patient. To this end, this article looks at the ocular manifestations of coronavirus (COVID-19): The Eye and Covid 19. It also explores the effect of covid 19 on the eyes.
Ocular Manifestation of SARS-CoV-2
Covid 19 became a global pandemic caused by a highly transmissible severe acute respiratory syndrome coronavirus 2 (SAR- CoV-2). This disease has been seen to affect the conjunctiva, the uvea tissues, and the retina and even extends towards neurological involvement. This may make the condition appear complicated. Redness, itches, and watery eyes are a few minor signs and symptoms which early infected patients may display.
The eyes face this risk due to a lack of eye protection with face shields as this virus is highly infectious. Ocular secretions are major transmitters of pathogens, thus care must be taken to ensure that the infected person and the non-infected persons are properly covered and guarded against making contact with these fluids. Although a significant effect has been noticed among animal species, the coronavirus has shown no marked effect on the eye for the human population. The noted effects in the human population include conjunctivitis, anterior uveitis, retinitis, vasculitis and optic neuritis.
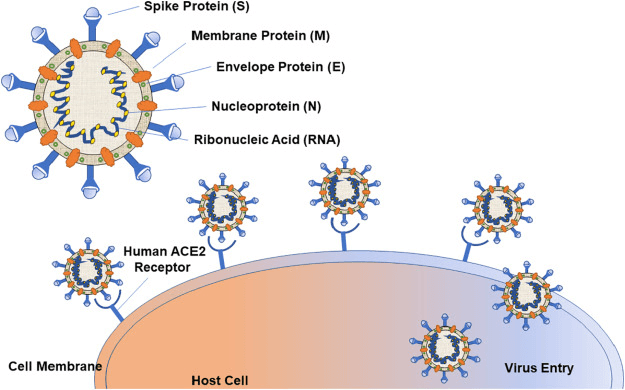
Pathogenesis of Corona Virus Infection
The pathogenesis and tissue tropism of SARS-CoV-2 relates to the binding of the viral spike protein to its cognate receptor on human host cells— the angiotensin-converting enzyme 2 (ACE-2) receptor. Efficient cell entry requires cleavage by protein transmembrane serine protease 2 (TMPRSS2). ACE-2 is expressed primarily on respiratory mucosal and alveolar epithelial cells and has been identified in other tissues, including the gastrointestinal tract, kidney, vascular endothelial cells, immune cells, and even neurons. Virulence is achieved via direct cellular invasion and death and the induction of widespread cytokine-driven inflammation and vascular leakage. Immune cell and complement debris can also lead to an increased thromboembolic state. This tries to explain the association between eye infection and covid 19.
The potential of infection through ocular secretions is currently unknown, and it remains unclear how SARS-CoV-2 accumulates in ocular secretions. Possible theories include direct inoculation of the ocular tissues from respiratory droplets or aerosolized viral particles, migration from the nasopharynx via the nasolacrimal duct, or even hematogenous spread through the lacrimal gland.
Symptoms of Covid 19 and the eye
- Eye redness
- Eye irritation and discharge
- Maybe watery or thick
- May be yellow, white, or green, and usually continues to drain throughout the day
- The affected eye often is crusty and stuck shut in the morning
- Irritation and discharge worsen for three to five days before improving, and symptoms can persist for two to three weeks
- Burning, sandy, or gritty feeling in one eye
- Cold symptoms
- Swollen glands (glands)
- Fever
- Sore throat
- Runny nose
Other symptoms of COVID-19 include:
- Shortness of breath
- Cough
- Fever or chills
- Muscle pain/body aches
- Changes in or loss of sense of taste and/or smell
- Headache
- Fatigue
- Sore throat
- Diarrhoea
- Nausea
- Vomiting
- Loss of appetite
- Congestion
- Runny nose
- Abdominal Pains
- Feeling unwell (malaise)
Eye pain and Covid 19

Eye pain in cases of covid 19 usually stems from the occurrence of conjunctivitis, episcleritis, scleritis or optic neuritis. This also presents with a headache and gets worse with increasing neurovirulence.
Symptoms of Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19
Conjunctivitis: Pink eye and Covid 19
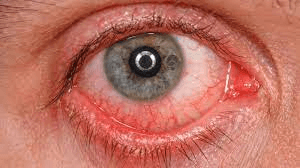
Pink eye and covid 19 have been associated with most patients suffering from coronavirus infection. Most covid 19 infected patients would present with acute conjunctivitis symptoms which include: eye redness, irritations, eye soreness, foreign body sensations, tearing, mucoid discharges, lid swelling, congestions and chemosis. Conjunctivitis oftentimes would not appear self-limiting in Covid-19 patients who present with it. Sometimes follicles and concretions are found around the palpebral conjunctiva. More so, there could be cases of hemorrhagic bilateral conjunctivitis with pseudomembrane formation Some corneal findings may present after 3 days of serious infection showing off transient pseudo-dendritic lesions and diffuse subepithelial infiltrates with overlying epithelial defects. It is important to note that in children or infants infected with the Covid 19 virus, there has been a strong association with a Kawasaki-like illness known as multisystem inflammatory syndrome in children (MIS-C). These kids have also shown cases of papilledema, iritis and keratitis.
How long does covid conjunctivitis last
Viral conjunctivitis (pink eye) usually lasts about one to two weeks, however, if it occurs in conjunction with COVID-19, other symptoms may persist longer, depending on the severity of the infection.
Scleritis/Episcleritis
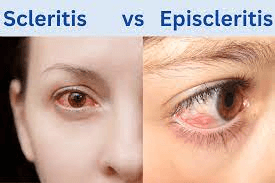
The past occurrence has shown cases of associated episcleritis, especially at the onset of the Covid 19 infection. Often times these are nodular episcleritis and necrotizing anterior scleritis.
Anterior Uveitis : an Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19
Cases of anterior uveitis have always occurred among covid 19 patients. There have also been cases of reactivated idiopathic anterior uveitis in post-covid 19 patients. Above all, individual cases of ocular infections should be handled independently but with the collective efforts of interdependent professionals.
Retinitis and Choroiditis in Covid 19
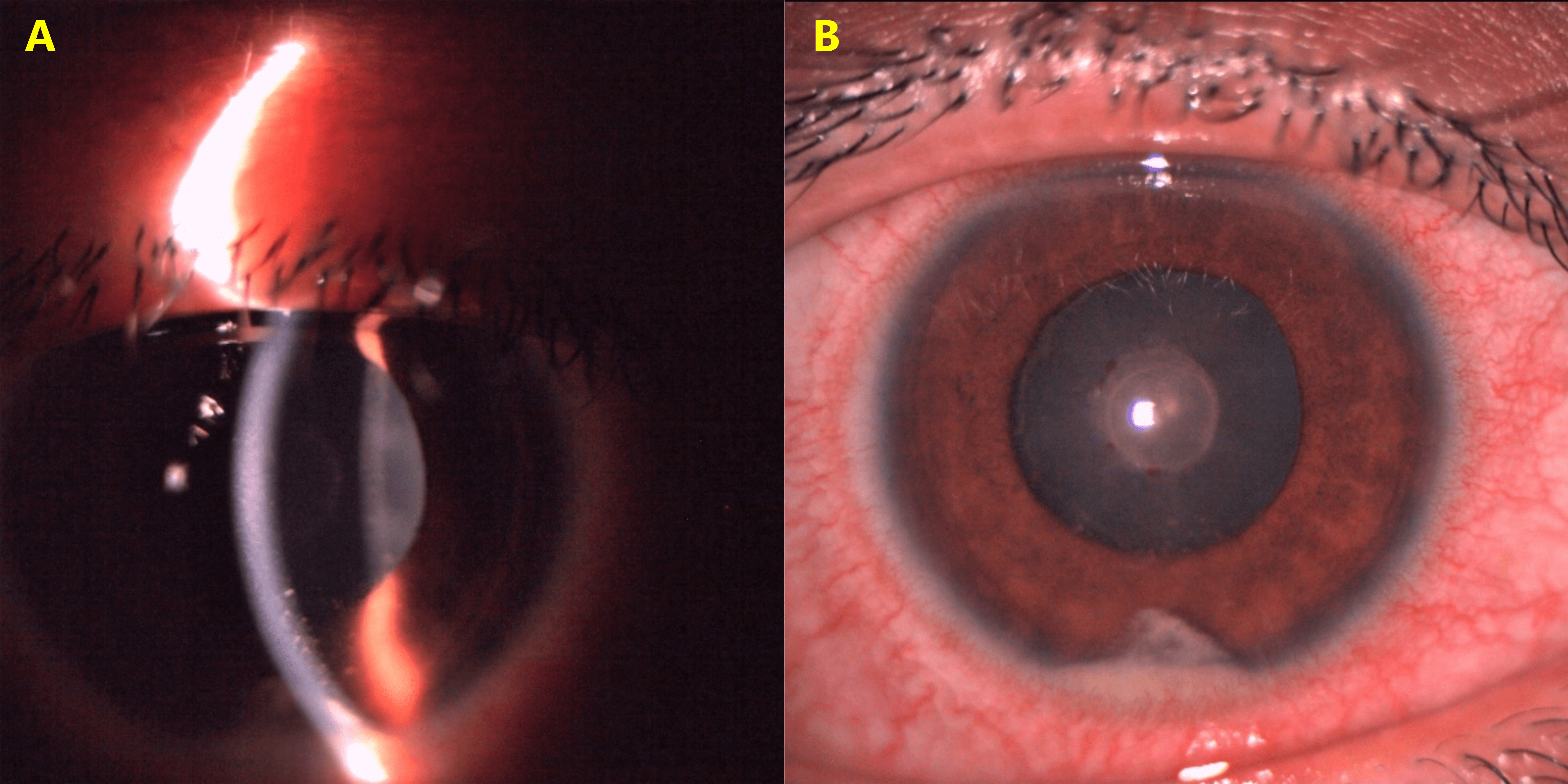
Posterior segment diseases have also been suspected to be associated with COVID-19 infection. These have varied between vascular, inflammatory, and neuronal etiologies. Both ACE-2 and TMPRSS2 are highly expressed in the human retina, and a recent case series of 3 patients discovered S and N COVID-19 proteins by immunofluorescence microscopy within retinal vascular endothelial cells, presumably containing viral particles. Eye floaters and covid 19 could be associated in some cases.
Both central retinal vein and artery occlusions have been reported in patients without classic systemic vascular risk factors. The hypothesized mechanism includes a complement-induced prothrombic and inflammatory state induced by the virus resulting in endothelial damage and microangiopathic injury. A striking example was reported by Walinjkar et al. with a central retinal vein occlusion (CRVO) in a 17-year-old female with COVID-19. Several cases of central retinal artery occlusions (CRAO) have been reported, potentially related to viral-induced endothelial insult and vasculitis.
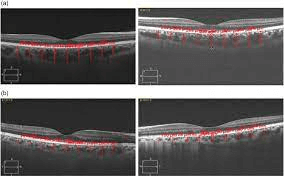
Acute macular neuro retinopathy (AMN) and paracentral acute middle maculopathy (PAMM), conditions in which there is ischemia to the deep retinal capillary plexus, have also been observed with COVID, marked by hyperreflective changes at the level of the outer plexiform and inner nuclear layers.
There have been reported cases of Purtscher-like retinopathy observed in patients with COVID-19. They presented with multiple bilateral cotton wool spots localized to the posterior pole after a month-long. Also, there is pneumonia associated with multiorgan failure and severe coagulopathy. Some patients present with bilateral areas of ill-defined retinal whitening and arteriolar narrowing following a severe COVID-19 infection associated with disseminated intravascular coagulation.
Optical coherence tomography (OCT) showed subclinical hyperreflective lesions at the level of the inner plexiform and ganglion cell layers in patients examined after systemic disease onset; cotton wool spots and microhemorrhages were found on dilated fundus examinations in these patients. It was also found that retinal vein diameter correlated directly with disease severity, suggesting that this may be a non-invasive parameter to monitor inflammatory response and/or endothelial injury in COVID-19. There are also several cases of choroiditis associated with Covid 19 infection.
Optic Neuritis and Covid 19
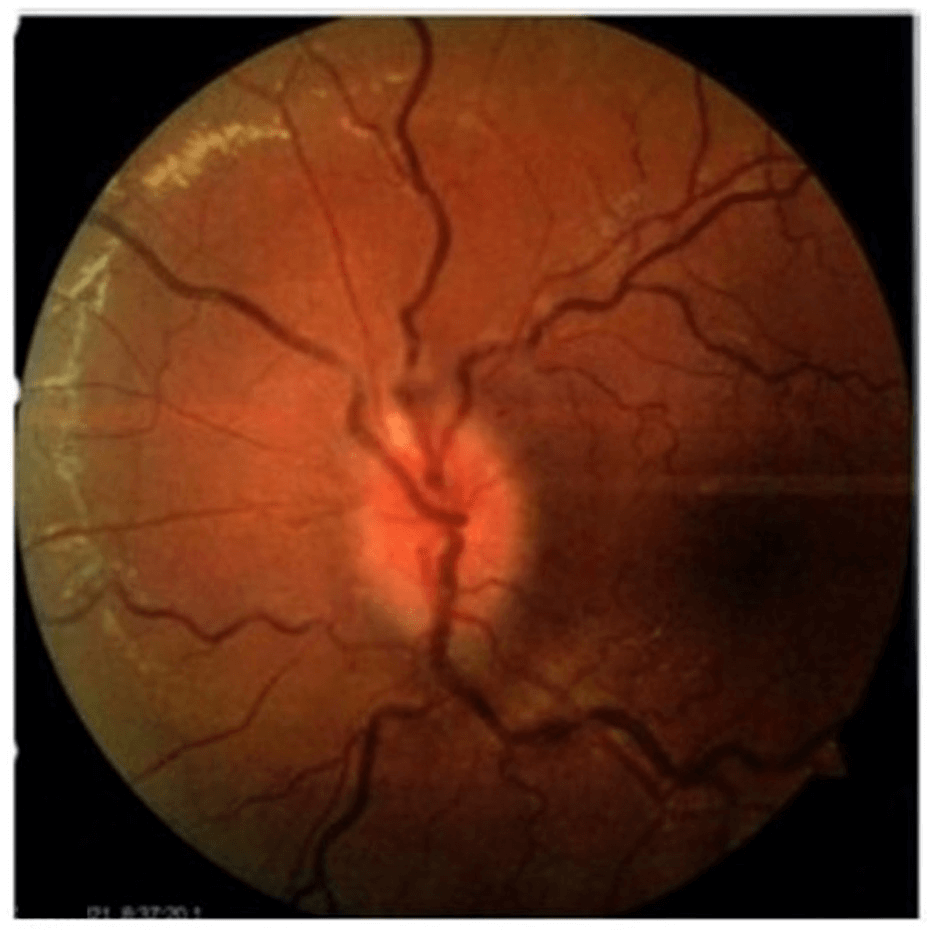
Optic nerve demyelination alongside other neuro-ophthalmologic manifestations has been seen in most cases of Covid 19 infections. While the mechanism has not been known, there has been suspected neuronal invasion, endothelial cell dysfunction leading to ischaemia and coagulopathy and/or widespread inflammatory cytokine storm induced by the virus. Optic neuritis has developed in several cases of the infected patients showing traces of neuromyelitis optica disorder and also the occurrence of anti-myelin oligodendrocyte glycoproteins (anti-MOG) antibodies. These patients present with subacute vision loss, a relative afferent pupillary defect, pain with eye movement, optic disc edema and radiographic findings of optic neuritis. Issues of optic neuritis also occur upon vaccination.
Extraocular Motility, Cranial Nerves
Cranial nerve III, IV, and VI palsies associated with COVID-19 have been reported within a few days of fever and cough onset, most without remarkable radiological features. Ocular cranial neuropathies and binocular diplopia with nerve enhancement on MRI have also been observed in association with post-infectious demyelinating conditions such as Miller Fisher and Guillain Barré syndrome. Patients were also found to have lower extremity hyporeflexia and ataxia consistent with Miller-Fisher syndrome.
Ocular myasthenia gravis has been described as a post-infectious sequela of COVID-19, with authors proposing that antibodies directed against SARS-CoV-2 proteins may cross-react with acetylcholine receptors and similar components at the neuromuscular junction. Huber and colleagues described a 21-year-old patient who presented 4 weeks after COVID-19 infection with fluctuating vertical binocular diplopia and ptosis, treated successfully with intravenous immunoglobulins and oral pyridostigmine.
Pupils
Pupillary changes have also been observed. Several groups have described patients with mydriasis and cholinergic super-sensitivity, indicative of tonic pupils and post-ganglionic parasympathetic pupillary nerve fibre damage.
Nystagmus
Oscillopsia has been reported in several cases of COVID-19 with neurologic involvement. Some patients have presented with intractable vertigo, nausea, and vomiting with a presumed diagnosis of viral-induced vestibular neuritis secondary to COVID-19. Central vestibular nystagmus has also been described in association with clinical and imaging findings consistent with rhombencephalitis.
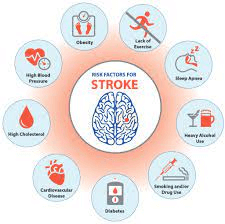
Visual Cortex
Perhaps the most devastating neuro-ophthalmic complication of severe COVID-19 infection is acute stroke affecting the posterior visual pathways. The incidence of stroke in these patients has been found to be 7.6 times higher than that of patients with influenza and has been occurring in a far younger-than-average patient population without classic vascular risk factors. These patients may present with homonymous visual field deficits prompting ophthalmologic consultation. There have also been cases of bilateral posterior cerebral artery ischemic strokes presenting as a homonymous visual field defect in infected children with multisystem inflammatory syndrome related to COVID-19.
Orbit and Ocular Adnexa in Covid 19
While oculoplastic and orbital manifestations of COVID-19 are uncommon, there is growing evidence to link inflammatory and infectious orbital disease to the virus. There have been reported cases of sinusitis, orbital cellulitis, and intracranial abnormalities in adolescents with COVID-19. It was postulated in this study at SARS-CoV-2 infection resulted in congestion of the upper respiratory tract and increased risk for secondary bacterial infection. This theory was expanded on by Shires et al., who reported a case of bacterial orbital abscess in a patient with COVID-19, with a unique intraoperative finding of highly avascular nasal mucosa and cultures positive for Streptococcus constellatus and Peptonipihilus indolicus, bacteria normally absent in the orbit or upper respiratory mucosa. It is possible that the local microbiologic and immunologic environment was altered due to avascularity induced by thrombosis in the setting of SARS-CoV-2 infection.
There have been a growing number of reports of acute invasive fungal rhino-orbital mucormycosis co-infection with COVID-19. These opportunistic pathogens thrive in the hypoxic respiratory environment induced by SARS-CoV-2, as well as an immunocompromised state induced by high-dose steroids and immunosuppressive therapies. In patients with poorly controlled diabetes, particularly those with diabetic ketoacidosis (DKA), the risk is further increased. Singh et al. published a systematic review of 101 reported cases of COVID-19 patients with mucormycosis; these patients were predominantly male (79%), 80% of which had diabetes and 15% with concomitant DKA. Corticosteroids had been used in 76% of these patients and nearly 60% of the cases reported rhino-orbital involvement. Another case described a 33-year-old female who presented with orbital compartment syndrome due to concurrent COVID-19 and fulminant mucormycotic infection.
There have also been reports of MRI-proven orbital myositis in two separate COVID-19 patients in the absence of concomitant bacterial infection. It was also postulated as either direct viral orbital invasion or induced autoimmunity as possible mechanisms.
Similar processes have been proposed by Diaz et al., who reported a case of acute dacryoadenitis in a 22-year-old male with positive SARS-CoV-2 antibodies who developed partial ophthalmoplegia. Other cases in this series include idiopathic inflammation in an anophthalmic socket.
Lacrimal System
Epiphora has been described as an initial finding in patients with COVID-19. This is thought to be secondary epiphora from inflammation of the conjunctiva. Direct involvement of the nasolacrimal system or the lacrimal sac has not been reported to date.
Evaluation of Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19
Case History
A thorough history is necessary regarding the onset, duration, and characteristics of symptoms. Anterior segment examination at the slit lamp or bedside can confirm findings of conjunctivitis or episcleritis.
Ocular examination
Measurement of visual acuity, intraocular pressure, and dilated fundus examination are warranted to rule out potentially more harmful ocular diseases. The clinician should perform a careful examination of pupils and colour testing to evaluate patients for evidence of optic neuropathy. Evaluation of extraocular motility may show evidence of nystagmus or cranial neuropathies. Visual field testing can detect and confirm deficits related to stroke.
Laboratory/Neurological Testing
SARS-CoV-2 can be detected in RT-PCR by sweeping the lower eyelid fornices to collect tears and conjunctival secretions with a virus sampling swab. Additional serum or cerebrospinal fluid testing may be useful to evaluate for inflammatory, autoimmune, or demyelinating entities. Neuroimaging can be valuable in patients presenting with optic neuritis, visual field deficits, and cranial neuropathies.
Differential Diagnosis
Ocular manifestations of COVID-19 have most commonly presented with conjunctivitis otherwise indistinguishable from other viral etiologies. Differential diagnosis includes a broad range of common ocular manifestations of eye redness and increased tearing:
- Other viral conjunctivitis (e.g., adenovirus)
- Bacterial conjunctivitis
- Allergic conjunctivitis
- Herpes simplex virus keratitis
- Anterior uveitis
- Corneal abrasion
- Foreign body
- Dry eye syndrome
- Exposure keratopathy in an intubated patient
- Chemosis in a critically ill patient associated with neurologic symptoms.
All patients should be questioned about recent fever, respiratory symptoms, exposure, and travel history to assess the need for further evaluation of COVID-19.
ALSO Read :
Prognosis of Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19
Conjunctivitis related to COVID-19 is currently thought to be self-limited. Larger studies and long-term follow-ups of patients with other ocular manifestations of COVID-19 have yet to be reported. Globally, we are in the grip of grim circumstances with ebbs and flows of infections. With the rather disjointed global response to the infection and unbalanced vaccine administration, the hope that out of the pain joy will spring and new strengths arise from recognition of the weaknesses of administrations around the world is a distant hope.
Below are some frequently asked questions on Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19.
FAQ
What can be done in eye and ear health emergencies during COVID-19?
• As part of a response to CoVID-19, there is scale back of routine health service provision in most health facilities.
• In case of critical eye or ear health emergency conditions such as sudden onset red eye or worsening ear condition, injury to eye or ears, sudden decrease in vision or hearing, severe pain in the eyes or ears and foreign body entry in eyes or ears; call the health care provider for consultation or for assessment.
Are people with preexisting eye or ear problems more likely to have COVID-19?
People with eye and ear problems are not more likely to have COVID-19 than the general population. Some NCDs such as diabetes, can have eye conditions as a manifestation of poor control. Those with pre-existing comorbidities such as diabetes, cancer, heart problems, chronic respiratory disease etc. are likely to have worse outcomes if they contract the virus.
• Many eye and ear health conditions are age-related and occur in older age groups. This age group have an increased likelihood of severe disease if they get COVID-19.
How can one prevent getting COVID-19 in an eye or ear health emergency?
Contact the health care provider via the phone for the condition to be assessed and be certain of the need to go to the health facility.
• Ensure adherence to social distancing of 1 meter.
• Consider using non-medical masks based on your risk assessment.
• Wash your hands frequently with soap and water or use an alcohol-based hand sanitizer if available. Always avoid touching your face.
How effective is remote consultation for eye and ear problems to avoid visiting health facilities?
It is effective to rule out an emergency eye or ear conditions through remote consultations.
• It is effective to get advice regarding the continuation of treatment for eye and ear conditions and follow-up.
• It is effective to get updated knowledge on COVID-19 and eye and ear problems.
What can be done in eye and ear health emergencies during COVID-19?
• As part of the response to CoVID-19, there is scale back of routine health service provision in most health facilities.
• In case of critical eye or ear health emergency conditions such as sudden onset red eye or worsening ear condition, injury to eye or ears, sudden decrease in vision or hearing, severe pain in the eyes or ears and foreign body entry in eyes or ears; call the health care provider for consultation or for assessment.
Are people with preexisting eye or ear problems more likely to have COVID-19?
• People with eye and ear problems are not more likely to have COVID-19 than the general population. Some NCDs such as diabetes, can have eye conditions as a manifestation of poor control. Those with pre-existing comorbidities such as diabetes, cancer, heart problems, chronic respiratory disease etc. are likely to have worse outcomes if they contract the virus.
• Many eye and ear health conditions are age-related and occur in older age groups. This age group have an increased likelihood of severe disease if they get COVID-19
How can one prevent getting COVID-19 in an eye or ear health emergency?
• Contact the health care provider via the phone for the condition to be assessed and be certain of the need to go to the health facility.
• Ensure adherence to social distancing of 1 meter.
• Consider using non-medical masks based on your risk assessment.
• Wash your hands frequently with soap and water or use an alcohol-based hand sanitizer if available. Always avoid touching your face.
How effective is remote consultation for eye and ear problems to avoid visiting health facilities?
• It is effective to rule out an emergency eye or ear conditions through remote consultations.
• It is effective to get advice regarding the continuation of treatment for eye and ear conditions and follow-up.
• It is effective to get updated knowledge on COVID-19 and eye and ear problems.
This article has tried to point out some salient points on: Ocular Manifestations Of Coronavirus (COVID-19): The Eye and Covid 19. This intends to help prevent cases of vision reduction from cases of corona virus infection on covid 19 cases.
ALSO Know some simple tips about your Health, Read below: