In the realm of post-stroke care, where patients face a complex web of health challenges, the importance of managing blood pressure effectively cannot be overstated. This critical aspect of recovery holds the potential to significantly impact the overall well-being and safety of individuals who have experienced a stroke. In this context, we delve into the intricate interplay between “Strategies for Effective Blood Pressure Control” and the pressing concern of “Minimizing the Risk of Falls” in post-stroke patients.
A stroke, a life-altering event, often leaves individuals vulnerable to a myriad of health issues, with the risk of falls looming large. Our focus here is on the promising prospect that lies in achieving better blood pressure control after a stroke. The keyword “reduce” takes center stage as we explore how meticulous management of blood pressure levels post-stroke may offer a potential lifeline, reducing the perilous risk of falls. Join us on this journey as we uncover the strategies, research, and insights that underpin this crucial facet of post-stroke care, shedding light on the intricate dynamics between blood pressure and fall prevention.
Let’s break down the statement:
- “Better blood pressure control”: This refers to the management and regulation of blood pressure levels in individuals who have had a stroke. Controlling blood pressure is a crucial aspect of post-stroke care to prevent complications.
- “After a stroke”: This indicates the specific time frame being considered, which is after someone has experienced a stroke. Stroke is a medical condition that can have various consequences, and post-stroke care is essential to minimize risks.
- “May reduce”: This is the key keyword in the statement. “May” suggests that there is a possibility or potential for a specific outcome. In this case, the outcome is the reduction of the risk of falling.
- “Risk of a fall”: This is the outcome being discussed. Falls can be detrimental, especially for individuals who have had a stroke, as they can lead to further injuries and complications.
So, the statement suggests that if blood pressure is effectively controlled in individuals after they have experienced a stroke, there is a possibility that the risk of falling could be reduced. However, it’s important to note that the use of “may” indicates that this is not a guarantee but rather a potential benefit that requires further research and clinical consideration.
- READ ALSO:
- Best Practice Materials for IELTS tests preparation 2023
- 2023 NNPC/Seplat Energy Internship for Undergraduate Students : APPLY NOW.
- Apply for the McCall MacBain Scholarships at McGill University
- FUNDED: Istanbul Kültür University International Awards 2023 For Undergraduate & Masters
- A Guide to Studying and travelling abroad
Post-stroke care is a complex and critical phase in the journey of stroke survivors. Stroke, a sudden disruption of blood flow to the brain, can have devastating consequences, often leading to physical and cognitive impairments. One significant challenge faced by post-stroke patients is the management of blood pressure. Elevated blood pressure, or hypertension, is not only a risk factor for stroke but also a potential complication after a stroke. It’s in this context that we delve into the strategies for effective blood pressure control to minimize the risk of falls in post-stroke patients.
Understanding the Post-Stroke Scenario

Before we delve into strategies for blood pressure control, let’s understand the post-stroke scenario. Surviving a stroke is a victory in itself, but it’s just the beginning of a challenging road to recovery. Stroke survivors often experience a range of physical and cognitive impairments, such as muscle weakness, balance issues, and memory problems. These factors increase the risk of falls, which can result in further injuries and complications.
The Link Between Blood Pressure and Stroke
To appreciate the significance of blood pressure control, we must first acknowledge the intricate relationship between blood pressure and stroke. High blood pressure is a leading cause of strokes, as it can damage blood vessels over time, making them more susceptible to rupture or clot formation. However, blood pressure management doesn’t stop once a stroke occurs.
Post-Stroke Blood Pressure Management
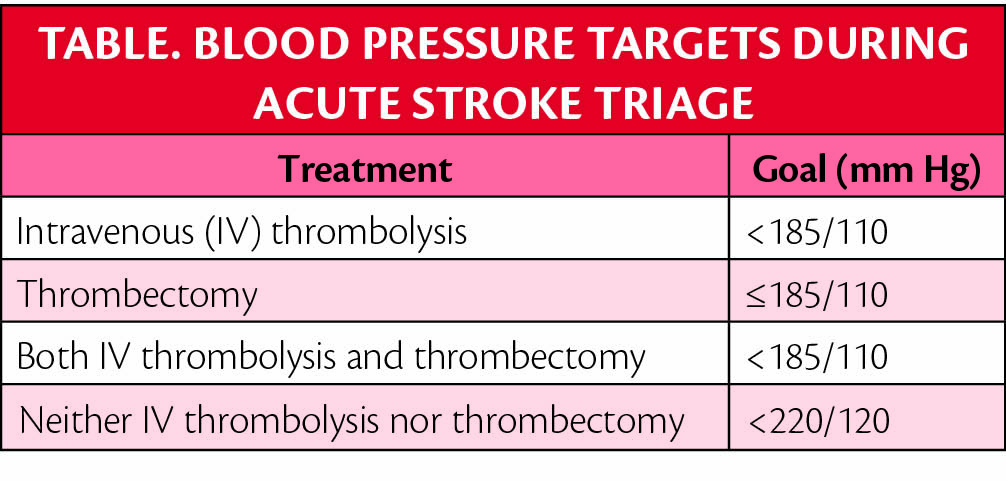
After a stroke, blood pressure management becomes a critical component of post-stroke care. The brain relies on a steady supply of oxygen and nutrients through blood circulation. When blood pressure is too high, it can strain blood vessels in the brain, potentially leading to a recurrence of stroke or other complications. Conversely, blood pressure that’s too low can deprive the brain of necessary oxygen, impairing recovery.
Strategies for Effective Blood Pressure Control

Now, let’s explore the strategies for effective blood pressure control in post-stroke patients, with a specific focus on how this can help minimize the risk of falls:
- Medication Management: Many post-stroke patients are prescribed medications to regulate blood pressure. Adhering to the prescribed medication regimen is crucial. It’s essential to take medications as directed and to communicate any side effects or concerns with healthcare providers.
- Lifestyle Modifications: Lifestyle plays a significant role in blood pressure control. Encouraging post-stroke patients to adopt a heart-healthy lifestyle can have a profound impact. This includes a balanced diet low in sodium, regular physical activity, stress reduction techniques, and avoiding smoking and excessive alcohol consumption.
- Regular Monitoring: Regular blood pressure monitoring is essential. Healthcare providers should monitor blood pressure during follow-up visits, but patients can also track it at home using home blood pressure monitors. This empowers individuals to be proactive in their care.
- Physical Therapy: Physical therapy is a vital component of post-stroke rehabilitation. It helps improve muscle strength, balance, and coordination. Enhanced physical fitness can reduce the risk of falls, indirectly aiding in blood pressure control.
- Fall Prevention Programs: Fall prevention programs specifically designed for post-stroke patients can make a significant difference. These programs often include exercises to improve balance and coordination, as well as strategies for making the home environment safer.
- Patient Education: Educating post-stroke patients about the importance of blood pressure control and fall prevention is crucial. When individuals understand the risks and benefits, they are more likely to actively engage in their care.
- Individualized Care Plans: Stroke recovery is not one-size-fits-all. Healthcare providers should develop individualized care plans that consider each patient’s unique needs, medical history, and risk factors. This personalized approach can optimize blood pressure control and fall prevention.
- Multidisciplinary Approach: Effective blood pressure control and fall prevention often require a multidisciplinary approach. This means that various healthcare professionals, including doctors, nurses, physical therapists, and occupational therapists, work together to provide comprehensive care.
The Impact of Effective Blood Pressure Control on Fall Prevention
Now that we’ve explored these strategies for effective blood pressure control, let’s examine the direct impact on fall prevention in post-stroke patients.
1. Improved Balance and Coordination: High blood pressure can impair blood vessel function, potentially affecting the brain’s ability to regulate balance and coordination. By controlling blood pressure, we can mitigate this risk, making falls less likely.
2. Enhanced Muscle Strength: Medications and physical therapy can help strengthen muscles, improving mobility and stability. This, in turn, reduces the risk of falls, which can have severe consequences for post-stroke patients.
3. Medication Side Effects: Some blood pressure medications can have side effects like dizziness or fainting. Proper medication management and monitoring can help mitigate these side effects, decreasing the likelihood of falls.
4. Cognitive Function: Hypertension can also impact cognitive function. Post-stroke patients who effectively control their blood pressure may experience better cognitive outcomes, reducing the likelihood of errors or lapses in judgment that can lead to falls.
What are the interventions for preventing falls in people post stroke?
Falls are a significant concern for individuals who have experienced a stroke. The aftermath of a stroke often includes physical impairments, such as muscle weakness and balance issues, which can increase the risk of falls. However, with the right interventions and strategies, it is possible to reduce this risk and improve the overall quality of life for post-stroke individuals. In this article, we will explore various interventions and techniques designed to prevent falls in people post-stroke.
Understanding the Risk Factors
Before delving into the interventions, it’s essential to understand the risk factors that contribute to falls in post-stroke individuals:
- Muscle Weakness: Stroke survivors often experience muscle weakness, particularly on one side of the body. This imbalance can make it challenging to maintain stability.
- Impaired Balance: Stroke can disrupt the body’s ability to maintain balance, increasing the risk of falling, especially when standing or walking.
- Visual and Sensory Impairments: Stroke can lead to vision problems or sensory deficits, which can affect a person’s spatial awareness and perception of the environment.
- Cognitive Impairment: Some stroke survivors may experience cognitive impairments, affecting their decision-making and awareness of potential fall hazards.
- Medication Side Effects: Medications prescribed after a stroke can sometimes cause dizziness or lightheadedness, making individuals more prone to falls.
Now, let’s explore the various interventions and strategies that can help mitigate these risk factors and prevent falls in people post-stroke.
- Physical Therapy:
- Physical therapy plays a pivotal role in improving muscle strength, balance, and coordination in stroke survivors.
- Therapists can design customized exercise programs to target specific weaknesses and help individuals regain their mobility.
- Occupational Therapy:
- Occupational therapists focus on enhancing a person’s ability to perform daily activities, such as dressing, cooking, and bathing.
- They can recommend adaptive strategies and equipment to make these tasks safer and more manageable.
- Home Modifications:
- Assessing the home environment is crucial. Simple modifications, such as installing grab bars in the bathroom and removing tripping hazards, can significantly reduce the risk of falls.
- Assistive Devices:
- Devices like canes, walkers, and orthotic braces can provide support and stability, making it easier for post-stroke individuals to move around safely.
- Depending on the patient’s assessed risk level, healthcare providers may implement various safety interventions, such as:
- Bed Alarms and Chair Alarms: These alarms are designed to alert healthcare staff when a patient attempts to get out of bed or a chair without assistance.
- Hip Protectors: These padded garments are worn to reduce the risk of hip fractures in the event of a fall.
- Non-Slip Footwear: Providing patients with non-slip socks or shoes can help improve their stability when walking.
- Bedside Rails and Grab Bars: Installing bedside rails on beds and grab bars in bathrooms can assist patients with balance and provide support during transfers.
- Floor Mats: Placing floor mats or cushions near the bedside or in areas where patients may fall can reduce the impact of a fall and prevent injuries.
- Medication Review:
- Regularly reviewing and adjusting medications with a healthcare provider can help minimize side effects that may contribute to dizziness or lightheadedness.
- Balance Training:
- Balance training exercises, like tai chi or yoga, can improve proprioception and enhance overall stability.
- Vision and Sensory Rehabilitation:
- Addressing vision and sensory impairments through specialized therapy or corrective devices can improve spatial awareness and reduce fall risks.
- Education and Awareness:
- Providing education to both the individual and their caregivers about fall risks and prevention strategies is essential.
- Encouraging the use of appropriate footwear and teaching strategies to get up safely after a fall can be valuable.
- Group Exercise and Social Support:
- Engaging in group exercise classes or support groups can boost motivation and reduce isolation, encouraging post-stroke individuals to stay active and maintain their balance.
- Regular Check-Ups:
- Scheduled check-ups with healthcare professionals can help monitor and manage any changes in health that may affect fall risk.
Preventing falls in people post-stroke requires a multifaceted approach that addresses the specific risk factors associated with stroke-related impairments. While it may not always be possible to completely eliminate the risk of falls, implementing the interventions and strategies discussed in this article can significantly reduce that risk and improve the overall quality of life for individuals on their road to recovery.
Stroke survivors, their families, and healthcare professionals must work together to create a safe and supportive environment that promotes independence and reduces the fear of falling, ultimately allowing post-stroke individuals to lead more fulfilling lives.
- More to read:
- MINIMUM SHARE CAPITAL REQUIRED FOR EACH COMPANY REGISTRATION
- Apply Now: Rhodes Scholarship 2024 to study at the University of Oxford |Fully-funded
- Full Scholarship 2024: PanAfrican University (African Union Commission) 2024.
- 20 Most current Undergraduate research topics in Public Health
Conclusion
In the complex journey of post-stroke care, effective blood pressure control emerges as a pivotal factor in minimizing the risk of falls. This interplay between blood pressure management and fall prevention highlights the holistic approach needed to ensure the well-being and safety of post-stroke patients. By embracing a combination of medication management, lifestyle modifications, regular monitoring, physical therapy, fall prevention programs, patient education, individualized care plans, and a multidisciplinary approach, healthcare providers can empower stroke survivors to regain control of their lives, reducing the risk of falls and enhancing their overall quality of life. In this endeavor, we strive for a future where post-stroke patients can enjoy a safer and more fulfilling existence on their path to recovery.
Join us on WhatsApp, Facebook and Telegram to receive Health & Scholarship alerts
